GCT – PATIENT INFORMATION SHEET
1.WHAT IS GIANT CELL TUMOUR??
GCT is a benign tumour that typically occurs in long bones. It has a potential for aggressive behaviour, high recurrence rate and capacity to metastasize. Although rarely it can spread to lungs and can be lethal.
2. WHY HAS IT OCCURRED TO ME??
There is no identified cause or known cause of giant cell tumour.
This is a rare tumour and affects 1 person in every 1 lakh people per year. And generally affects those aged 20 to 45 years of age.
3.HOW TO DIAGNOSE GIANT CELL TUMOUR??
STEPS TO DIAGNOSE-
A. BLOOD INVESTIGATIONS-
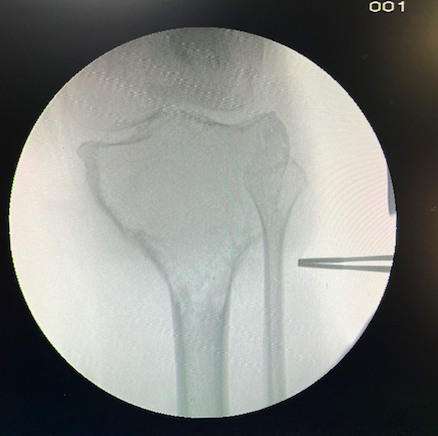
B.X RAY- to see the affected bone and size of the tumour
C. MRI- to see any soft tissue involvement
D.CT THORAX- to rule out lung metastasis
D. BONE BIOPSY- part of the disease is removed to check under microscope to confirm the disease. A procedure where a doctor places a small needle through the skin and into the lesion to withdraw a sample of the abnormal tissue. The tissue is analysed to confirm any findings.
4.STAGES OF GCT
Staging and grading are used to describe the severity of the disease. Staging is based on the following things
- Location of tumour
- Size and extent of the tumour
- Whether cancer cells have spread to lymph nodes or anywhere else in the body.
- The number of tumours present.
Doctors use tumour grade, cancer stage, and a patient’s age and general health to decide the course of treatment for the patient and determine prognosis. Prognosis describes all factors including the disease course, cure rate, chances of survival, and risk of recurrence of cancer.
5. WHAT IS TREATMENT PLAN??
The main aim of treatment is to remove the tumour, while maintaining as much of the cosmetic
appearance and functional normality of the bone as possible.
A. MEDICAL
Medical management has been utilized preoperatively to reduce the tumour size, diminish the tumour’s blood supply, and facilitate joint preservation procedures in periarticular locations.
Also it hardens the tumour which makes the surgery easy and reduces surgery related complications
Fresh Blood investigations are needed before each round of treatment.
1)ZOLENDRONIC ACID– given once a month , usually for 3 months
2) DENOSUMAB -usually given once a week initially then biweekly.
B.SURGICAL
1)EXTENDED CURRETAGE WITH CEMENTING-GCTs are benign yet locally aggressive tumours, a local intralesional surgical approach is deemed appropriate in most cases. Curettage surgery involves the removal of the tumour by scraping the tumour cells from the area. This procedure is commonly followed by ‘bone cementation’ – which aims to destroy any remaining tumour cells and fill the area following the tumours removal. Treatment include Curettage, extensive pulse lavage, application of hydrogen peroxide, heat cauterization and cementing with bone cement.
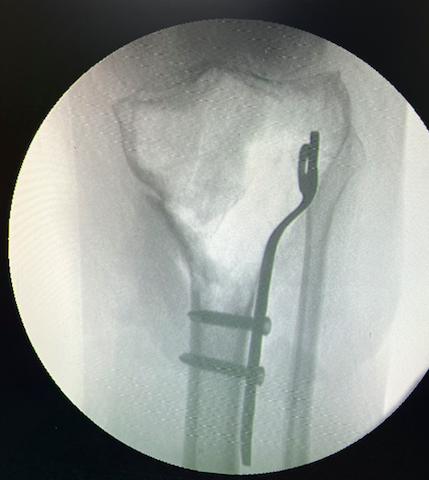
2)RESECTION– Resection may be the preferred option in benign tumours, particularly when bone salvageability through intralesional methods would cause a severe compromise in mechanical characteristics. This applies particularly to the “expendable bones,” such as the lower ulnar and upper fibular end, where excision may be the treatment of choice.
3)RESECTION AND RECONSTRUCTION-Used in extensive cases where the cortex has been breached and replacement is the only option available. In cases of GCT in the distal radius, resection and reconstruction with an allograft or an autograft are commonly undertaken.

7.WHAT COMPLICATIONS CAN OCCUR??


- Tumour recurrence- most common complication
- Osteoarthritis of the knee joint
- Stress fracture
- Limited movement
- Pulmonary metastasis
- Local and deep infections
- Osteomyelitis
- Joint degeneration
8. WHAT IS MY PROGNOSIS??
Early detection and treatment often leads to better outcomes .
GCT have a favourable prognosis and after good physiotherapy patients get good range of motion and no pain. Main complications that can occur and lead to poor prognosis are recurrence and lung metastasis.
9. WHAT IS MY FOLLOW UP SCHEDULE?
Follow ups are important to identify the complications like recurrence and metastatis.
After operative management patients usually need follow up every 3 month initially for routine check ups for routine X rays and CT scan of Thorax. Then after 2 years , patients are usually called 6 monthly for the same investigations.
10. WHAT ARE MY SURVIVAL CHANCES??
The survival rate for GCT patients is very good. The five-year recurrence-free survival rate is around 80-91% for both benign and malignant GCT.
